Flap surgery is a common dental procedure primarily used to treat advanced periodontal (gum) disease. When the gums have receded and pockets of infection have formed around the roots of the teeth, nonsurgical methods like scaling and root planing may no longer be effective. In these cases, flap surgery allows a dental professional to gain access to the root surfaces and bone, clean them thoroughly, and restore healthy tissue attachment. This article explores flap surgery in detail, its purpose, procedures, benefits, risks, and post-operative care.
What Is Flap Surgery?
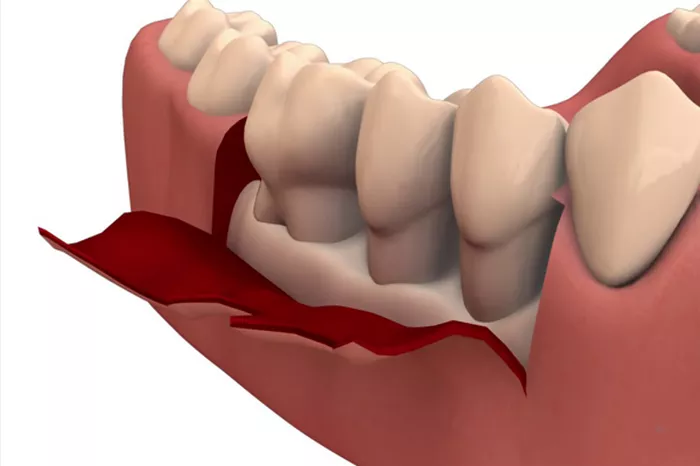
Flap surgery is a periodontal procedure used to treat advanced gum disease by exposing the roots of the teeth and surrounding bone. During the surgery, the gum tissue is carefully lifted to allow thorough cleaning of tartar and bacteria from deep pockets that cannot be reached with regular cleaning. This process helps eliminate infection, reduce pocket depth, and promote healing, ultimately aiming to preserve the teeth and restore gum health.
Why Flap Surgery Is Performed
Flap surgery is indicated when nonsurgical periodontal treatments have failed or when the disease is too advanced for those methods to work effectively. Some of the main reasons for performing flap surgery include:
Deep periodontal pockets that cannot be cleaned with scaling and root planing alone
Severe gum inflammation that persists even after nonsurgical treatments
Bone loss that needs to be evaluated and possibly regenerated
Gum recession that affects tooth stability and aesthetics
In essence, flap surgery is often a last resort to save teeth that would otherwise be at risk due to extensive periodontal disease.
The Anatomy of the Periodontium
To fully grasp the significance of flap surgery, it’s helpful to understand the anatomy of the periodontium—the supporting structures of the teeth. These include:
Gingiva (gums): The soft tissue that surrounds the teeth and covers the bone.
Periodontal ligament: The connective tissue fibers that anchor the tooth root to the bone.
Alveolar bone: The bone that contains the tooth sockets.
Cementum: A calcified layer covering the tooth root, anchoring the periodontal ligament.
Flap surgery primarily targets the gingiva and alveolar bone, helping restore their function and structure when compromised by disease.
Types of Flap Surgery
There are several types of flap surgery depending on the specific goals of the treatment. These include:
1. Modified Widman Flap
This technique involves minimal reflection of the gum tissue to allow access for root debridement while preserving as much tissue as possible.
2. Full-Thickness Flap
Also called a mucoperiosteal flap, this involves lifting the entire soft tissue and periosteum from the bone surface to gain maximum access to the roots and bone.
3. Partial-Thickness Flap
Only a part of the gum tissue is reflected, typically used when preserving periosteal blood supply is critical, especially in regenerative procedures.
4. Papilla Preservation Flap
This approach is used in esthetic areas to maintain the interdental papilla and avoid the formation of black triangles after surgery.
The Step-by-Step Procedure of Flap Surgery
Understanding what happens during flap surgery can help patients prepare for the procedure both mentally and physically. Here is a breakdown of the surgical steps:
Step 1: Anesthesia
Local anesthesia is administered to numb the treatment area, ensuring the patient experiences no pain during the surgery.
Step 2: Incision
The surgeon makes small incisions in the gum tissue to create a flap. This allows them to gently lift the gums away from the teeth and bone.
Step 3: Cleaning and Debridement
The exposed roots are cleaned of plaque and tartar deposits using manual and ultrasonic tools. The surgeon may also smooth irregular bone surfaces to discourage bacterial growth.
Step 4: Bone Reshaping or Grafting (if needed)
If there is significant bone loss, the surgeon may reshape the bone or place bone grafts to encourage regeneration.
Step 5: Flap Repositioning and Suturing
Once the area is clean and any grafts are placed, the flap is repositioned and sutured back into place to promote healing.
Step 6: Postoperative Dressing
A periodontal dressing may be placed over the surgical site to protect it and reduce discomfort.
Postoperative Care and Recovery
Proper care after flap surgery is essential to ensure successful healing and long-term periodontal health. Patients should follow these guidelines:
1. Oral Hygiene
Patients are usually advised to avoid brushing the surgical area for several days. Instead, they may use antimicrobial rinses like chlorhexidine to keep the area clean.
2. Medications
Antibiotics may be prescribed to prevent infection, and pain medications or anti-inflammatory drugs can help manage discomfort.
3. Diet
Soft foods are recommended for at least a week post-surgery. Hot and spicy foods should be avoided to prevent irritation.
4. Follow-Up Visits
Patients typically return for suture removal and to monitor healing within 7 to 10 days after the procedure.
Benefits of Flap Surgery
Flap surgery offers several significant advantages for patients with advanced periodontal disease:
Reduction in pocket depth to make future cleaning easier and more effective
Removal of bacterial toxins that can harm bone and soft tissue
Preservation of natural teeth by stabilizing the periodontium
Improved esthetics in some cases, especially when tissue grafts are used
Risks and Complications of Flap Surgery
While generally safe, flap surgery does come with some risks, including:
Infection at the surgical site
Swelling and bruising in the operated area
Post-operative bleeding, usually minor and self-limiting
Tooth sensitivity, especially to hot and cold
Gum recession leading to exposed roots
Flap Surgery vs. Scaling and Root Planing
Flap surgery is often compared with scaling and root planing (SRP). The primary difference lies in the level of invasiveness and the severity of the disease treated.
Scaling and root planing is a non-surgical procedure used in early to moderate periodontal disease.
Flap surgery is reserved for more advanced cases where pockets are too deep to be cleaned non-surgically.
SRP may be performed prior to flap surgery as an initial step in the treatment plan.
Alternatives to Flap Surgery
Not every case requires flap surgery. Depending on the severity and progression of periodontal disease, alternatives may include:
Antibiotic therapy using localized delivery into the gum pockets
Laser periodontal therapy for shallow to moderate pockets
Periodontal maintenance for long-term disease control without surgical intervention
Patient Selection and Candidacy
Not all patients are good candidates for flap surgery. Ideal candidates include those with:
Moderate to severe periodontitis with deep pockets
Good systemic health to support healing
Commitment to oral hygiene and follow-up care
Contraindications include uncontrolled diabetes, smoking, and immunocompromised conditions, all of which may affect healing and outcomes.
Conclusion
Flap surgery is a powerful tool in the management of advanced gum disease. By giving access to deep pockets and infected bone areas, this surgical method provides an opportunity to restore oral health, preserve natural teeth, and prevent further deterioration. While it comes with some risks, the benefits often outweigh the drawbacks, especially for patients at risk of tooth loss due to periodontal disease. Consulting with a periodontist and understanding the full scope of the procedure ensures that patients make informed decisions tailored to their unique dental health needs.
Related topics