Oral health suffers from a chronic image problem. It is too often perceived as an afterthought or a purely cosmetic concern, a stark contrast to how society approaches heart disease. Public health campaigns, early screenings, and aggressive preventive measures dominate the conversation around heart health, while dental issues remain largely sidelined. This disparity is largely due to the immediate and sometimes deadly consequences of heart disease, such as heart attacks and strokes, compared to the slower, less visible progression of oral health conditions like cavities and gum disease.
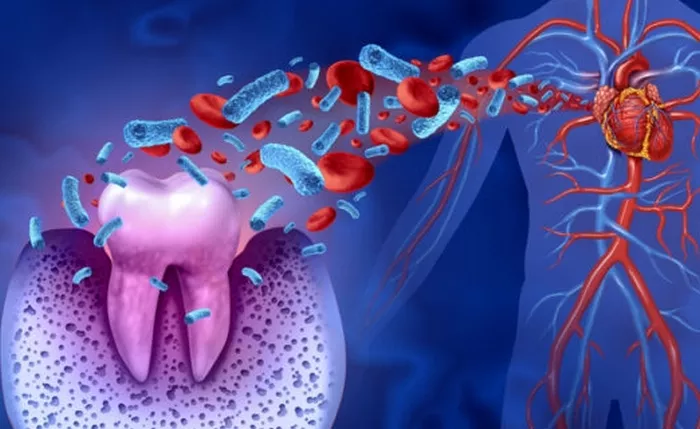
Yet this slower development of dental diseases contributes to a dangerous misconception that they are not serious — merely uncomfortable rather than threatening. However, oral infections are strongly linked to serious conditions such as heart disease, complications from diabetes, and even brain infections. Furthermore, the indirect consequences are staggering: emergency room visits, lost school hours, and decreased workplace productivity. In the United States alone, these hidden costs exceed $45 billion annually, and children miss 34 million hours of school because of dental-related issues.
To truly improve national health outcomes, dental care must be addressed with the same rigor and urgency as chronic disease prevention. Preventive care should be seen not only as essential medical practice but also as sound public policy. A critical first step is expanding access to preventive dental coverage.
Currently, only 73% of U.S. adults have dental insurance — a stark contrast to the broader reach of health insurance. Out-of-pocket costs also make up a disproportionate share of dental expenses. In 2024, these costs accounted for 40.3% of total dental spending, far surpassing the 10.6% of total health spending. This financial burden is largely driven by Medicare’s exclusion of dental benefits. As of 2019, nearly 24 million Americans — roughly 47% of all Medicare beneficiaries — lacked dental coverage. While some individuals find partial relief through Medicare Advantage plans, these tend to offer limited benefits.
Without insurance, adults are over twice as likely to say they cannot afford dental care. This financial inaccessibility results in markedly higher rates of severe dental issues, including 8.5% with severe tooth loss, 14.3% with severe periodontitis, and 37.9% with untreated cavities. This gap in preventive care drives up the number of dental-related emergency room visits. Between 2005 and 2016, approximately 11% of avoidable ER visits were for dental problems that could have been addressed with regular care.
Encouraging more people to seek routine dental checkups begins with making that care more affordable and accessible. But financial access alone is not enough. To create lasting change, public education about the seriousness of oral health is essential.
Many people see dental appointments as little more than a routine cleaning, failing to recognize their role in screening for chronic disease. The belief that dental visits are only necessary when there’s visible pain is a deeply rooted misconception. In reality, early intervention is as critical in dental care as it is in addressing cancer or heart disease. The earlier a condition is detected, the better the outcome.
Research shows that greater health literacy leads people to better understand their oral health and communicate more effectively with their providers. When people are informed about the consequences of poor oral hygiene, they are more likely to adopt regular dental care habits. As with preventive screenings for cholesterol or blood pressure, public efforts should offer free dental evaluations and wide-scale educational campaigns to inform the public.
At the same time, data must be collected to measure the effectiveness of these educational efforts. Just as researchers track cardiovascular risk and screening data, oral health interventions should be monitored to identify gaps in access and understand what motivates individuals to prioritize their dental health.
Another overlooked factor is the classification of oral care products in financial planning systems. The IRS currently categorizes floss, toothpaste, and mouthwash as general health products, similar to shampoo, which makes them ineligible for Flexible Spending Accounts (FSAs) and Health Savings Accounts (HSAs). This policy reflects a fundamental misunderstanding of the preventive value of these products.
A bipartisan effort in Congress seeks to change that. The proposed Oral Health Products Inclusion Act (H.R. 8599) would make essential oral hygiene items eligible for FSA and HSA reimbursement. Since these products are instrumental in preventing cavities and gum disease, such a change would represent a major step forward in making preventive dental care more accessible and affordable. Like most healthcare interventions, preventive strategies in oral health reduce treatment costs and boost productivity.
The nation has made great strides in addressing heart disease through systematic and integrated approaches. If similar efforts were applied to oral health — through expanded insurance, education campaigns, and better access to preventive products — the result would be a healthier population and billions in savings. But that change will only come when dental health is recognized not as optional, but as an integral part of overall health.
Related topics